EY refers to the global organization, and may refer to one or more, of the member firms of Ernst & Young Global Limited, each of which is a separate legal entity. Ernst & Young Global Limited, a UK company limited by guarantee, does not provide services to clients.

Contributors:
Rachel Simmons, Manager | Business Consulting - National Health Practice, EY Canada
Lauren Monardo, Senior Manager | National Healthcare Practice, EY Canada
Breaking down silos and putting humans at the heart of strategy can lead to a sustainable transformation of Canada's primary care system.
In brief
- Investing to improve Canada’s primary care system enables patients to access more appropriate care more quickly, leading to better health outcomes all while dialling down strain on the system.
- To achieve those outcomes, health system stakeholders must first dismantle silos and commit to working together over the short and long term.
- Investing funding and strategy in this process now can generate significant return on investment in the years ahead, but those investments must encourage sustainable change practices that keep those affected at the centre.
Good primary care is at the heart of a well-functioning health system. Canadian leaders and provincial authorities are increasingly seeking to transform primary care systems in support of better long-term health outcomes. But for this kind of large-scale change to succeed, it must be grounded in the actual needs of real stakeholders. That means putting humans — from the front-line physicians to everyday patients — at the heart of a strategy that is equal parts innovative and practical, and doing so now.
What obstacles are holding primary care transformation back in Canada?
The short answer? Silos. Across Canada, the outcry for health system improvements has hit a persistent fever pitch among patients, clinicians, and staff. Primary care is commonly cited as a priority area for modernization.
What are people looking for? Quicker access to — as well as better quality and continuity of — care, when and where it’s needed most. Meaningful, team-based care that is truly collaborative and interprofessional, not just co-location by another name. Integrated, patient-centred care journeys that bring care closer to home. And naturally the funding to go with it.
Among these stakeholders, we hear a growing consensus that team-based care models are the best way out of our workforce challenges and are capable of supporting better health outcomes well into the future. For these models to succeed, they require an integrated, connected and coordinated framework of primary care services grounded in:
- The promotion of a wellness-based system focused on prevention and social determinants of health, including the alignment of funding and payment mechanisms for ensuring high-quality care and reaching desired health and system outcomes.
- Locally planned and centrally accountable service provision driven by population health data, including the engagement of patients and communities in co-designing care and models of participatory care.
- Continuous quality improvement and innovation backed — but not hindered — by the latest technology, including the use of information and communication technologies to enhance access and quality, and the implementation of performance measurements and quality improvement systems.
We’re already seeing some of these factors influence health care for the better. For example, increased, meaningful and sustainable adoption of artificial intelligence (AI) and digital solutions is growing across the sector.
The trouble is, much of this progress is happening in silos or isolated pockets, or never progressing past the pilot stage. To really get at system transformation and improve access to quality care across a population — and, over time, better health outcomes — these incremental changes must be much more connected overall.
As well, a general lack of centralized leadership in primary care has led to the emergence of different stakeholders with competing priorities that do not necessarily align precisely to federal or provincial strategic plans. But people must work together to scale this kind of change outside of stakeholder spheres of influence.
To succeed, primary care transformation requires cooperation and involvement between the health sector, educational institutions, unions, professional associations, municipalities, housing, infrastructure, innovation and economic development. It also necessitates long-term, reliable funding, which has traditionally been hard to come by in primary care, as well as meaningful commitments to frontline workers, who are increasingly burned out and fatigued by waves of change and piecemeal or temporary solutions.
This kind of transformation is absolutely a long game requiring upfront investments. The real return on investment isn’t likely to be noticed in the short term, but rather in the sustained and significant savings achieved over 10 to 15 years. Today’s investments enable the kind of proactive health care that improves outcomes and reduces strain on the system.
Overcoming these barriers will undoubtedly require strong political will — something that’s beginning to take hold. But forging the kind of lasting change health care needs now requires a systematic, deliberate and integrated approach to transformation that marries willingness to change with practical steps for delivering on this potential.
How can Canada’s health care system successfully transform primary care?
At EY, we help health systems in Canada and around the world transform by first and foremost putting humans at the centre of the change. Research carried out collaboratively between the EY organization and the University of Oxford shows that giving specific focus to a series of human factors can increase the probability of transformation success to more than 70%.
What does that mean in the primary care context? Clinicians, managers, and frontline staff must understand what tomorrow looks like, how their daily workload could be improved and how they’ll be held accountable for changes. What’s more, the changes themselves must be developed with key system users in mind — including patients — for transformation to work.
This humans at centre focus is our jumping off point. From there, we work through a four-stage process of design principles to help transform health systems. This includes:
1. Strategic planning during which stakeholders come together to define the future state of the health system and desired outcomes.
2. Preparing and piloting the change, which begins with an honest assessment of existing infrastructures and how they may enable or limit progress towards the future-state vision.
3. Scaling transformation across the system, expanding pilot activities across the entire system and geography of the transformation.
4. Sustaining transformation over time, closing the gap with the future state through targeted and focused initiatives, phasing out old policies, tools and mindsets that are incongruous with the new normal.
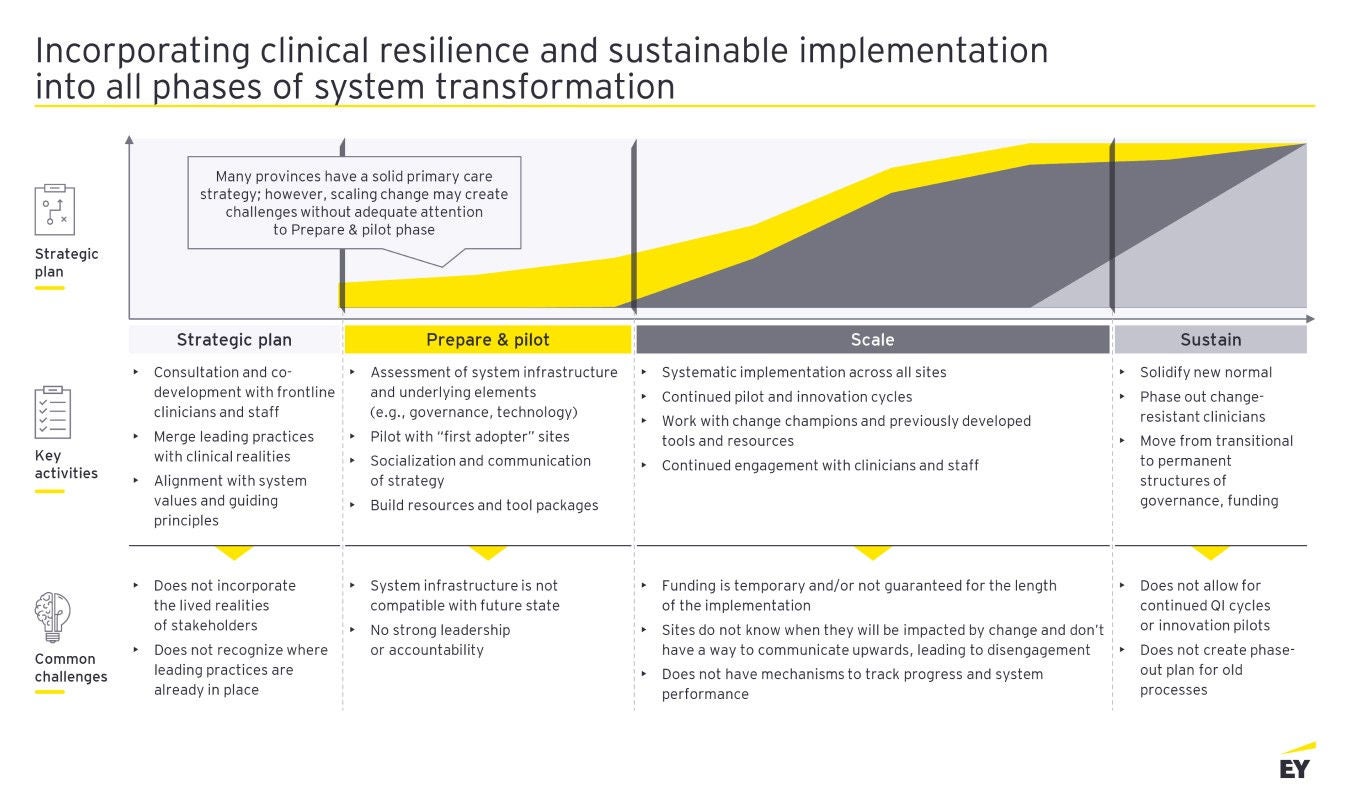
When it comes to primary care, each stage is meant to include practical steps that enable seamless flow to the next. Unfortunately, there is often an uneven distribution of attention and resources put on the first and second phases. Time and time again, we see the thoughtful engagement of frontline staff and primary care experts in strategic development, but then quick, almost rushed progress through the preparing and piloting phase, particularly given public pressure for change.
Many health systems do not continue taking advantage of the stakeholders and champions who are already engaged in the transformation process or put enough thought into systemic barriers and underlying requirements that may impede successful scaling of change.
That said, weaving the point of view of frontline clinicians and patients into subsequent phases will surface additional considerations or resources required for future phases. For example:
1. Access to team-based and interprofessional models of care using a wellness-based approach. This may mean protected time and space for interprofessional meetings and learner exposure to these environments, regular coverage mechanisms that both clinicians and patients can rely on, incentivized processes for team-based care and team members dedicated to prevention activities.
2. Appropriate use of communication and information technologies that support an integrated, connected and coordinated primary care system. This may include digitizing archives, teaching clinicians, staff and patients how to use effectively digital tools, transitioning multiple stakeholders over to single electronic medical records (EMR) or health records, administrative time on task reduction and redistribution, appropriate updates and improvement cycles to EMRs.
3. Value-based systems that align accountability metrics and funding to health outcomes and addressing social determinants of health. This may include appropriate task distribution to full scope of practice, training for mental health and other wellness and social determinants of health services, clear lines of accountability, different leaders who echo the same messaging, and primary care-specific KPIs for health outcomes and value-based care.
4. Engagement of patients and communities in planning local service delivery, driven by easily accessible population health data. This implies access to quality data, decision-making processes that incorporate population health data, managing resistance to change from older solo practitioners, changing practice expectations, and community and municipal service integration.
Related content
Six ways to make more of AI in Canadian health care
What health care organizations do to seize the potential of generative AI could unleash possibilities improve health outcomes for years to come. Learn more.
Summary
Dismantling silos and blending strategy and practicality into a framework for change, such as this, makes transformation possible. What’s more, because the system for change is reverse engineered to the specific needs of health care stakeholders, working in this way also makes transformation exciting, sustianable and agile. These factors are crucial to successfully changing the system — and health outcomes — for the better, in this increasingly complex environment.