Chapter 3: Co-Creating the Future: Patients’ Role in AI-Driven Healthcare
Patients and users are becoming more actively involved in the healthcare evolution, participating in the development of drugs, devices and digital platforms. This trend is driven by an ethical imperative but is also a strategic business move, making clinical trials more patient-centric, considering users’ preferences in medical device development and involving patients in shaping digital health technology as well as telemedicine platforms. This involvement helps in developing products that meet real-world needs, potentially improving health outcomes, adoption and patient satisfaction. Companies are establishing patient engagement programs and advisory boards to incorporate patient feedback directly into the development and testing processes, ensuring devices meet actual patient needs. Moreover, the emphasis on patient-centered outcomes by regulators highlights the importance of this trend across the healthcare sector.
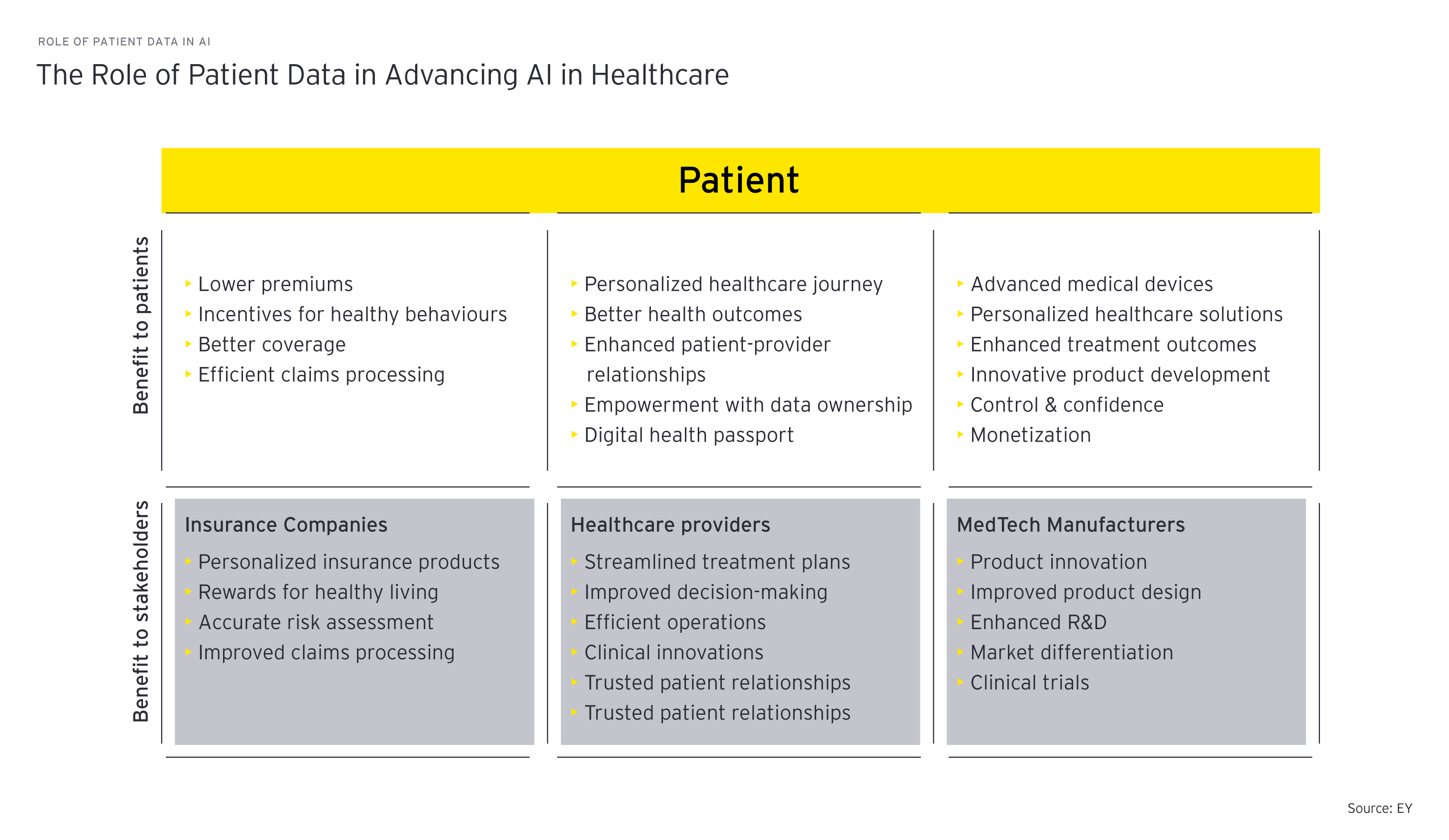
AI development in MedTech could benefit from users’ involvement, not only as feedback for algorithm improvement or usability and adoption, but also in particular from a data perspective. Involving patients ensures a more ethical design process, where the rights and concerns of patients are addressed immediately. Trust is a significant barrier to AI adoption in healthcare, and involving patients in the creation and validation of AI tools can foster a greater sense of trust and increased adoption.
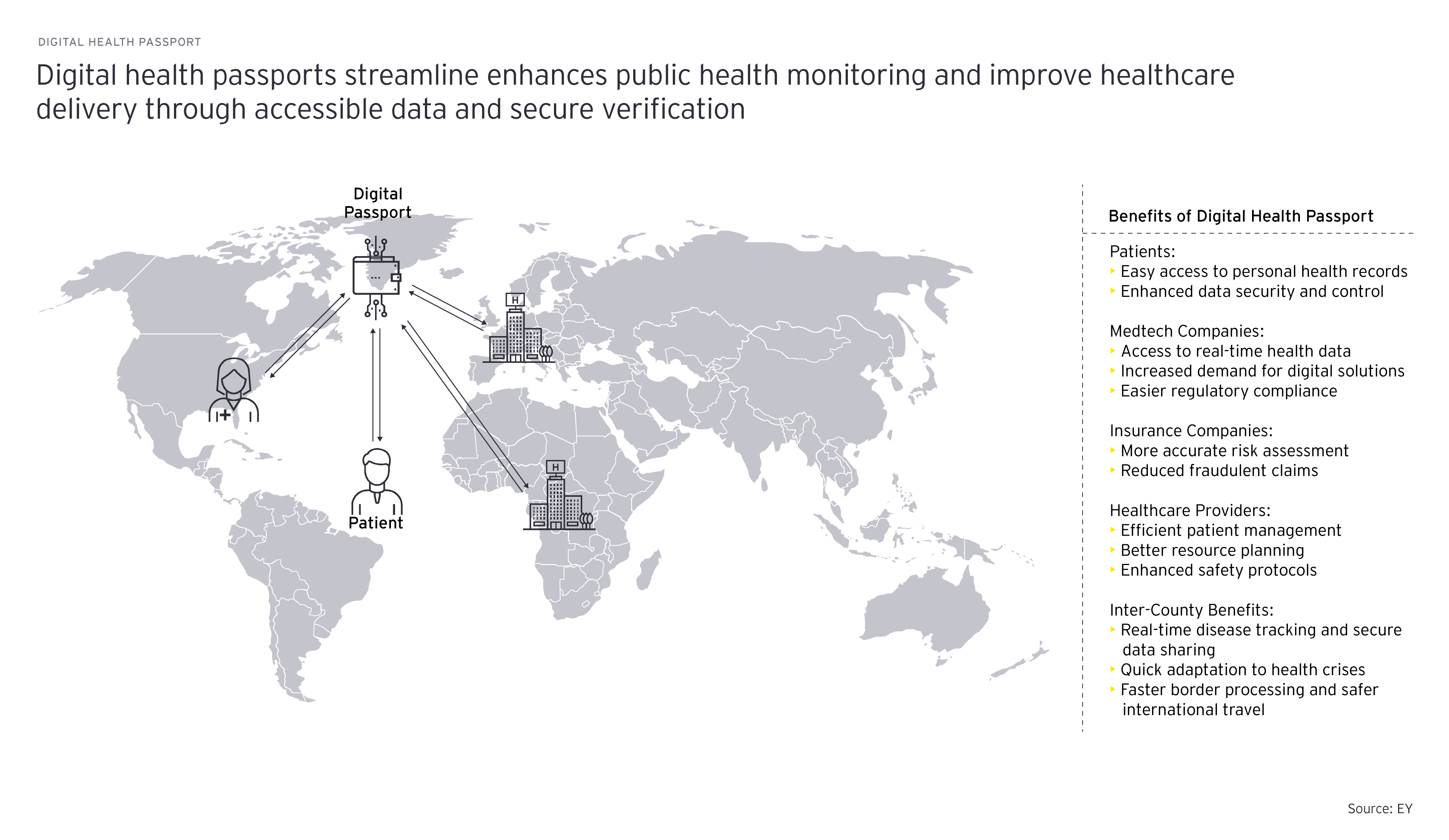
Due to the lack of control over which data is being gathered and how and the obfuscation of how that data is being used, data ownership is a heated debate. By data ownership we mean that patients have legal rights and control over their own health-related data. This implies that patients have the primary authority over who can access and use their data, including the ability to grant or revoke access to their data for healthcare providers, researchers or payers (a matter of consent). It also encompasses the right to transfer their data between different healthcare providers, insurance companies or health information systems, and to maintain ongoing oversight on fair use and the benefits derived from the use of their data. This concept of data ownership should ensure the mobility of a patient’s data, enabling it to seamlessly follow the patients as they travel or move, ensuring continuity of care across borders or different healthcare systems without compromising data privacy or control over their data.
Empowering patients by granting data ownership is easier said than done. Many patients, particularly those who are older or less technologically savvy, may struggle to comprehend the full extent of what they consent to, the intricacies of data usage in complex research endeavors or the functionality of their own digital health passports. This gap in understanding necessitates a robust and accessible educational framework that simplifies these concepts without diluting their significance. By granting patients ownership rights over their own data, companies recognize patients’ autonomy and the value of their data. Companies can build even deeper trust, thus further breaking down barriers to AI adoption. When patients have assured control over their data and the possibility to decide where their own data is being used and how, they are more likely to share it and provide accurate and up-to-date information. This will lead to higher quality and real-world data, ensuring that AI models are better trained and more representative (EY Consumer Health Survey). Data ownership can promote the transition of patients from passive subjects to active contributors, fostering long-term relationships where patients continually provide data, feedback and insights. Monetization for patients could involve receiving compensation or benefits for their active participation and data contribution, or enhancing the value they receive from the healthcare ecosystem.
Providers can benefit from access to comprehensive health history and high-quality, real-world data that reflects actual patient needs and outcomes as well as enables personalized and more efficient care plans. Moreover, when patients are in control of their data, they are more likely to trust their healthcare providers. This trust fosters a more open patient-provider relationship, encouraging patients to share crucial health information. The challenge lies in adapting to an information system where patients control their data, requiring providers to navigate consent issues and data portability seamlessly. For providers, monetization could come from offering premium services or leveraging the comprehensive data to improve patient care and reduce costs, potentially leading to better health outcomes and increased patient satisfaction.
Insurance companies traditionally rely on health data to assess risks, set premiums and manage claims. Patient-owned data could significantly alter how insurers access and use health information, presenting them with both challenges and opportunities. On the one hand, if patients control their data, insurers might face difficulties in accessing comprehensive health records for risk assessment without explicit consent, potentially leading to new models for risk calculation and premium determination. On the other hand, this scenario could encourage insurers to develop more personalized insurance products and wellness programs that reward healthy behaviors and proactive disease management with strong focus on prevention. Insurers could also benefit from more accurate data directly from patients, leading to more effective healthcare spending, better risk management and fraud prevention. Monetization for insurers could involve creating personalized insurance plans and health programs that utilize patient level data to incentivize and reward healthy lifestyles, thereby attracting more customers and reducing costs.
Medtech manufacturers, including those producing medical devices, wearables and diagnostic equipment, are increasingly integrating digital technologies into their products, generating vast amounts of data. By recognizing patients’ autonomy and the value of patient generated data, manufacturers can build deeper trust and break down barriers to AI adoption. If patients own their data, manufacturers may need to develop more sophisticated consent mechanisms and data-sharing agreements to access and use this data for product improvement or research purposes. However, this shift also opens opportunities for manufacturers to differentiate their products through patient centric features such as secure data portability, interoperability with other health systems and personalized healthcare solutions based on patient data analytics. Collaborating with patients in this way could lead to innovations in product design and functionality as well as stronger patient trust and loyalty. The operational challenge is in creating infrastructure that supports data portability and secure sharing, aligning with patient consent. Monetization for manufacturers could come from offering advanced, data-driven products and services that command a premium in the market, as well as from the potential of using patient data to drive innovation and efficiency in product development.
By supporting data ownership, regulators can ensure that patients’ rights are central to healthcare innovations, promoting a healthcare ecosystem that values privacy, consent, and patient autonomy. Establishing clear guidelines for data ownership and patient consent helps create a stable regulatory environment that encourages innovation while protecting patient interests. Moreover, clear, patient-focused regulations can increase public trust in healthcare systems and technologies, encouraging more people to participate in digital health initiatives and share their data for research. However, developing regulations that accommodate the fast pace of technological advancements in healthcare while protecting patient-centric data is challenging. Creating regulations that allow for the cross-border flow of health data, necessary for global health initiatives, while ensuring that data protection standards are met, presents legal and logistical challenges. Regulators must balance the need for data protection with the need for innovation and efficiency in healthcare, ensuring that regulations are not overly burdensome while still protecting patients. Monetization for regulators could involve creating and enforcing certification programs or data compliance audits that ensure adherence to data protection standards, potentially generating revenue through certification fees.
IT providers play a critical role in developing technologies for data portability, secure sharing and interoperability. They can position themselves as leaders in healthcare innovation by aligning with regulators to establish privacy and security standards as well as patient engagement practices. There is potential for strategic partnerships across the healthcare sector to develop holistic solutions for data ownership and portability challenges. However, creating infrastructure for the secure and efficient exchange of patient data between various systems presents technical hurdles, demands regular updates and necessitates international interoperability and standardization. Ensuring top-tier data security and privacy, with stringent measures against breaches and unauthorized access, is crucial and demands continuous innovation. Developing systems that are interoperable, not only within a country’s healthcare system but also internationally, is a significant challenge, necessitating collaboration and standardization across the industry. Ensuring the highest standards of data security and privacy, including robust protection against data breaches and unauthorized access, is paramount and requires constant vigilance and innovation. Monetization for IT providers could come from offering subscription-based platforms, charging for the use of proprietary software that facilitates data exchange or providing consulting services to healthcare organizations navigating the complexities of data portability and security.
The shift towards patient involvement and data ownership in healthcare represents a transformative movement, addressing the ethical imperative for patient autonomy and presenting strategic advantages across the healthcare sector. From enhancing clinical trials to shaping the development of medical devices and digital health platforms, this approach fosters products that align with actual patient needs, improving health outcomes, adoption rates and satisfaction. Recognizing patients’ legal rights over their health-related data not only empowers them but also sets a foundation for trust, a crucial element in the widespread adoption of AI in MedTech. However, realizing this vision involves overcoming challenges, such as bridging the knowledge gap for patients, ensuring seamless data portability as well as maintaining rigorous data security and privacy standards. Together, stakeholders across the healthcare industry must collaborate to overcome the technical, legal and ethical challenges presented by patient data ownership, paving the way for a more patient-centric, transparent and effective healthcare system.