EY refers to the global organization, and may refer to one or more, of the member firms of Ernst & Young Global Limited, each of which is a separate legal entity. Ernst & Young Global Limited, a UK company limited by guarantee, does not provide services to clients.

Openness to new health technologies and digitally enabled pathways of care provide an opportunity to reshape patient experience and improve health outcomes.
In brief
- Care models are shifting out of the hospital and into the home, but patient data exists in silos preventing integrated care pathways. A new information architecture can address this.
- Disruption of traditional care models with AI will lead to a shift to more personalised and preventative healthcare services.
- Openness to non-traditional channels of care delivery and use of wearables highlights patients’ desire for more accessible healthcare.
Faced with a growing ageing population, prevalence of chronic diseases, rising healthcare costs and increasing clinician workforce shortages, health systems must transform to remain sustainable. The EY Global Consumer Health Survey 2023 highlighted the need for improvement in the performance of health systems which, despite record spending, still face significant challenges. On the other hand, the survey also indicated the openness of people to digital health transformation, providing an opportunity to reimagine care delivery to drive better outcomes for all.
Here are five ways we can create a more integrated model of care:
1. Embed digital across all health and care settings
Any organisation that designs a system will produce a design whose structure is a copy of the organisation’s communication structure.
Within many healthcare systems we typically see communication structures involving lots of handover between different teams working in different organisations — such as a hospital, GP, or local authority. The result of this is a digital health system that is built around individual organisations with lots of data integration required to try and follow the patient as they move between care settings.
This situation exemplifies Conway’s law in action — how health and care organisations communicate reflects how information is used and shared by health IT.
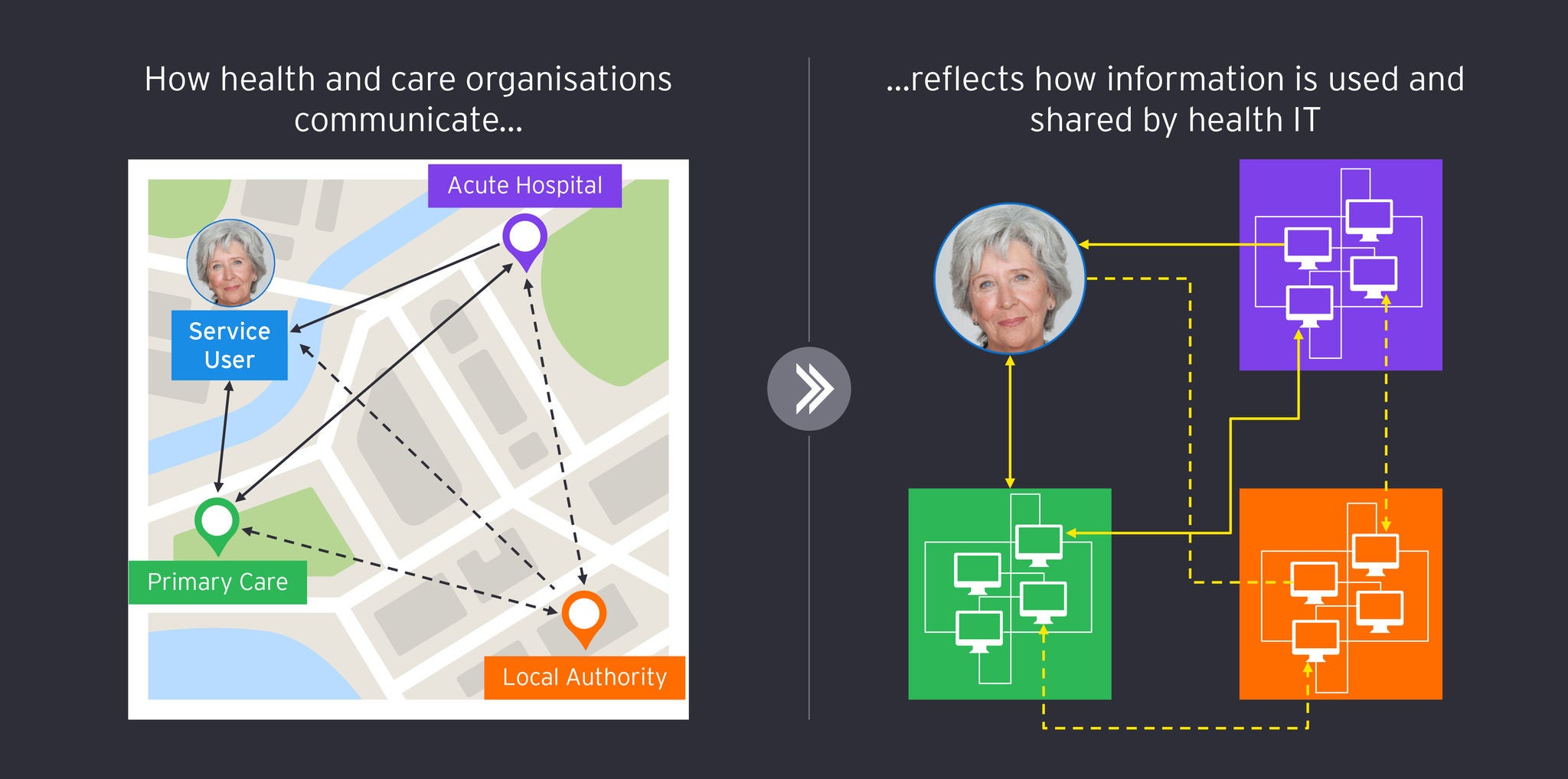
To support new care-delivery models we must shift away from this organisation-first approach and design systems that are centred around the person.
2. Adopt a patient-centred approach to data
In the world of healthcare technology, the phrase "patient centred" has become something of a mantra. You are unlikely to witness any presentation or talk by a health IT vendor not claiming to be patient centred. Yes, individual applications may have functionality centred around a patient, but when considered together and in the context of the patient pathway, are they actually “patient centred”?
I’m reasonably sure if you asked most patients they would say “no”, given it is they who must navigate the complexities of the organisation-centred approach illustrated above.
Achieving patient-centred care is not something an individual application can solve on its own. Regardless of your digital health strategy there will always be multiple applications that co-exist across the system. To ensure these applications do not exist in siloes with fragmented data that is difficult to access or share, a new information architecture is required. This architecture will:
- Ensure the patient record is stored separately from any individual application, allowing any application to access and utilise the record;
- Model and share the record using open healthcare standards and specifications, including FHIR, openEHR and IHE;
- Establish trust through robust security and privacy controls, that are defined at the data level, alongside appropriate clinical governance and streamlined data sharing agreements;
- Be an integral part of a broader transformation program with a robust interoperability strategy, active vendor community alignment, and supportive legislation in place to foster adoption.
This approach is already being adopted across many countries, including:
- London: The NHS in London has deployed a patient-centred platform across five integrated care systems, 40 NHS trusts and 1,400 general practices enabling Londoners to have their care information shared digitally city-wide with both patients, and health and care professionals.
- Catalonia: For providing integrated care, the National Health System of Spain is creating a longitudinal electronic health record on a platform based on openEHR covering eight million citizens and 60 hospitals.
- Slovenia: Slovenia has deployed a national interoperability backbone, based on FHIR, openEHR and IHE, which collects patient data in an open, structured and vendor-neutral format connecting more than 2.1 million patients across 35 hospitals and 57 primary care centres.
3. Provide intelligent services that are simple to use
Despite rapid innovation in the last 10-15 years in areas such as cloud, mobile working and AI, most clinical applications used today are built using outdated 90s concepts, with lots of windows, menu options, dialog boxes and complex forms to capture information. Studies1 have shown that the impact of this poor design and the associated documentation burden are leading causes of clinician burnout.
AI is perceived as critical to transforming care delivery, creating intelligent digital experiences that are more personalised and simpler to use. 52% of the healthcare industry acknowledge that AI will be commonly used in the next 10 years (EY Consumer Health Survey 2023), and it is easy to understand why, with a range of AI-powered use cases set to revolutionise the clinician-patient experience.
For example, ambient listening technology can listen (with consent) to clinician-patient interactions in real time. Such a system can auto-generate clinical notes, capturing the essence of the consultation without the clinician having to manually enter data. This not only reduces the documentation burden but also allows clinicians to focus more on patient care. Furthermore, AI-powered co-pilots, where the AI supports clinicians, suggesting inputs and streamlining the data-capture process based on the context of the patient-clinician interaction. This approach could significantly reduce the time and effort involved in data entry while improving data accuracy.
Amidst this potential, the healthcare sector stands out for its complex relationship with AI. The industry oscillates between the enthusiastic anticipation of AI’s potential to improve patient outcomes, and cautious scepticism — especially regarding the ethical, privacy, and regulatory implications involved. Developing AI ethically and responsibly will be key to supporting this transformation, using models that are open, explainable, and integrated with trusted sources of patient information.
4. Personalised healthcare where and when it’s needed
In the EY Global Consumer Health Survey 2023 ‘access to care when needed’ was one of the key priorities for respondents. In Ireland, one of the six countries surveyed, 63% valued that the most from the healthcare system.
Global results also indicated a strong openness to non-traditional care delivery such as using non-traditional channels for routine appointments (66%) and being treated by a hospital-at-home programme (60%). Irish respondents, in particular, demonstrated a strong interest in the use of wearables with 70% stating they would allow one to collect and transmit data versus the 64% global average. They also were in favour of genetic testing (71%), use of a retail clinic for non-urgent care (68%), treatment via a hospital-at-home programme (61%) and would be open to taking medication personalised for their genetic profile (64%).
Hospital-at-home programmes have already been adopted in many countries including Ireland. One example is the CARE project in Donegal, a community virtual ward, which is reducing hospital admissions for patients with COPD.
Global research into hospital-at-home care highlights its benefits:
- Australia has recorded 36 fewer hospital visits per 100 patients over 12 months as part of a remote dialysis programme.
- A Mount Sinai study in the US, found a difference of $4000 in acute care costs between that of a hospital-at-home approach compared to inpatient treatment. This was based on total costs for the acute episode and the 30 days after.
- A reduction in patient suffering has been shown, with those in hospital-at-home care spending less time lying down, requiring significantly less lab work, and far fewer patients needing readmission within 30 days compared to that of inpatients
5. Deliver user-centred outcomes
In the ongoing transformation of healthcare towards a more patient-centred, integrated model, technology certainly plays a pivotal role. Yet it's important to recognise that successful transformation is not merely a matter of implementing the right technology. It encompasses various critical aspects, including change management, governance, privacy safeguards, and resource allocation.
While each of these aspects is extensive and could warrant its own in-depth discussion, it's evident that strong leadership at all levels is crucial to navigate this transformation successfully. Importantly, this leadership must ensure that future digital health services as not seen as IT projects with technical outputs, but instead strategic products that deliver outcomes for their users.
For example, rather than having a system that can measure the inflammatory biomarkers for a certain cohort of patients over 70 years old (an output), we should be building systems that measure how many people within this cohort are able to achieve their lifestyle goals, such as walking to the local shop (an outcome).
Successful projects tend to be those that maintain a laser focus on the outcome they are trying to deliver and the problem they need to solve for their users. Adopting this approach often has the added benefit of allowing a thinner vertical slice of functionality to be delivered sooner, in contrast to trying to build an entire horizontal layer of technology, all of which may not be required to solve the problem.
Summary
To deliver fully integrated care, digital transformation is key. With people keen to embrace new forms of health technology as well as a willingness to share data, what’s needed is a clear framework that enables health settings to communicate easier, harnesses the power of data and positions the patient experience at its centre. By connecting people, technology and data in this way we help deliver effective, personalised care with improved outcomes.



