EY se refiere a la organización global, y puede referirse a una o más, de las firmas miembro de Ernst & Young Global Limited, cada una de las cuales es una entidad legal independiente. Ernst & Young Global Limited, una compañía británica limitada por garantía, no brinda servicios a los clientes.
Cómo EY puede ayudar
The voice of the clinician also must be incorporated. “As care models and clinical journey maps are designed as a part of the product development process, it is important to remember there are two customers: the clinician as well as the patient or consumer. We need to simplify the workflow to minimize clinician burnout and think about how we can make their lives easier using clinical decision support tools, AI and machine learning (ML), while also getting into the life flow of consumers to make sure that we are building something that is simple to use and gets their needs met,” said Kristi Henderson, Senior Vice President and CEO, Optum Everycare, during an EY webcast on virtual care. “While digital can be anywhere, we really have to build trusted relationships, so it’s really important to invest in that. If you’re going to have a digital or virtual PCP, be intentional about engagement and high-value touch points to allow those trusted relationships to occur,” she said.
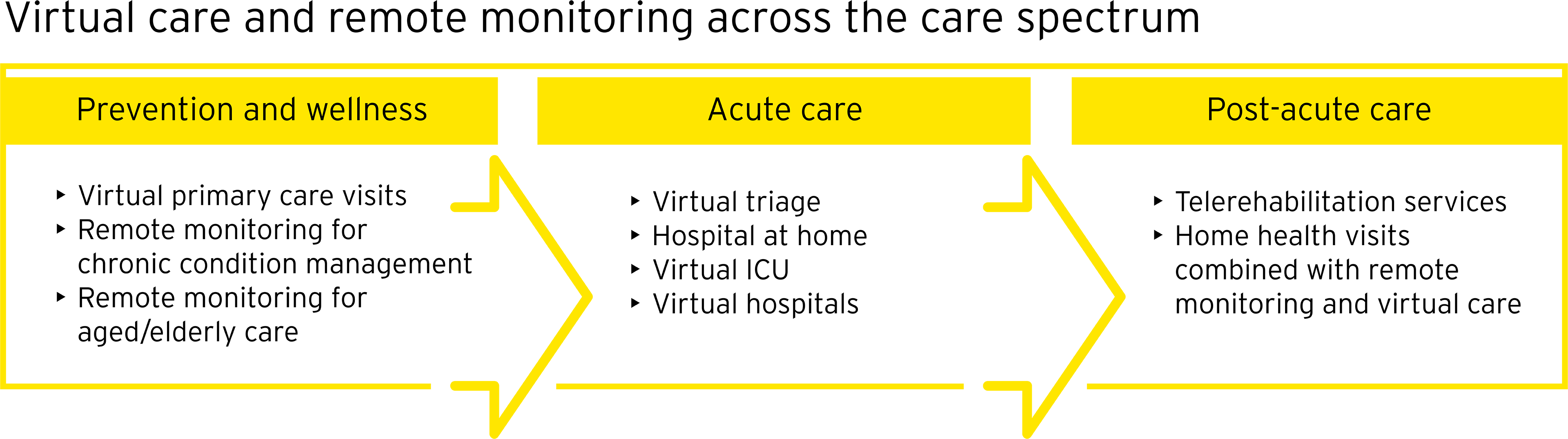
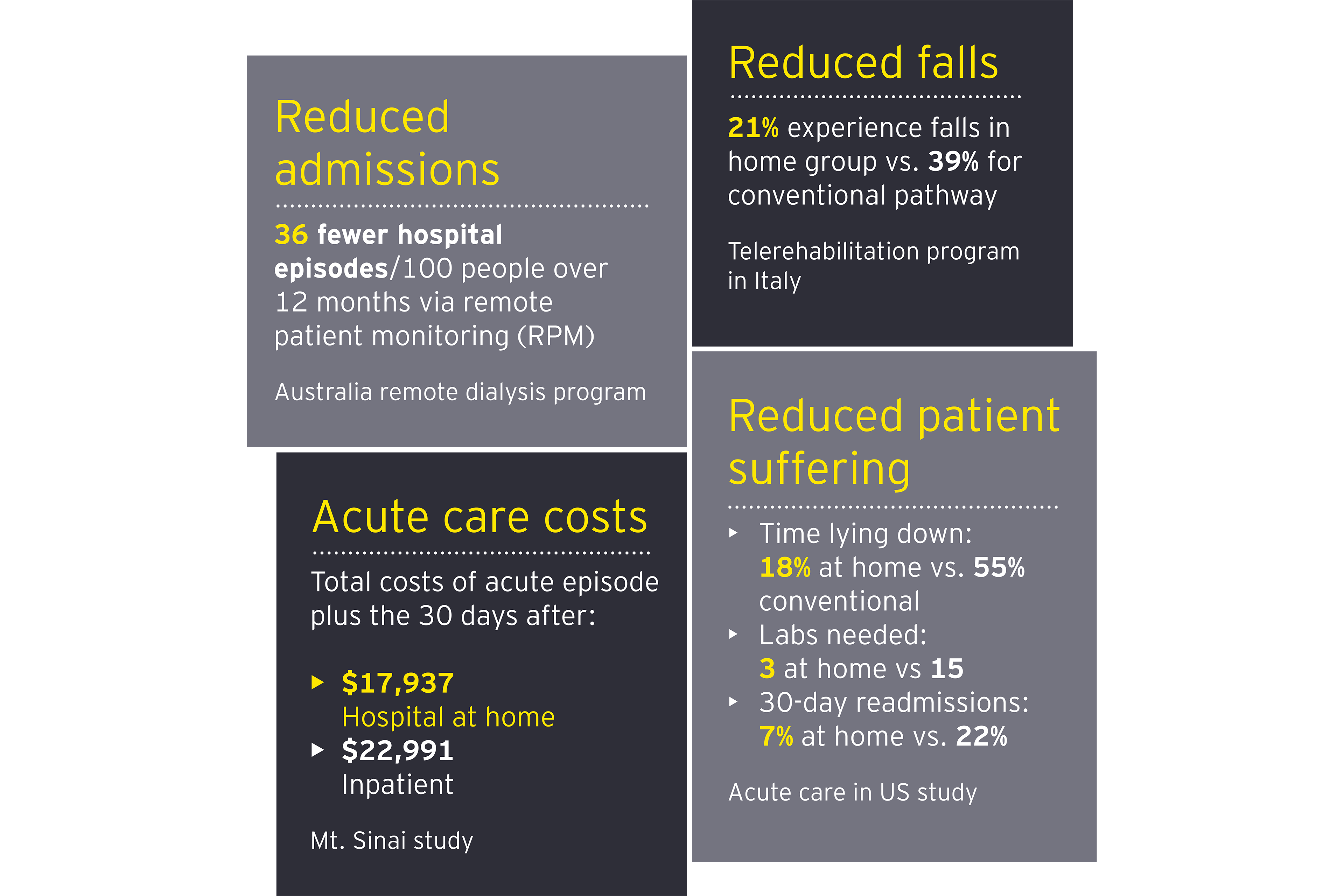
Health care organizations and ecosystem partners continue to invest in virtual and remote care models with the global telehealth and telemedicine market expected to grow from $87.8 billion in 2022 to $285.7 billion by 2027.10 In the US, Mayo Clinic and Kaiser Permanente have partnered to deliver acute care at the home with Medically Home, which estimates that 30% of hospitalized patients can benefit from the model.11 Retail giants Best Buy and CVS have recently invested in their own virtual care platforms.12 The UK and Singapore are expanding their use of virtual wards for certain medical conditions, while Israel has opened a virtual hospital.13
Where can health organizations make the shift now?
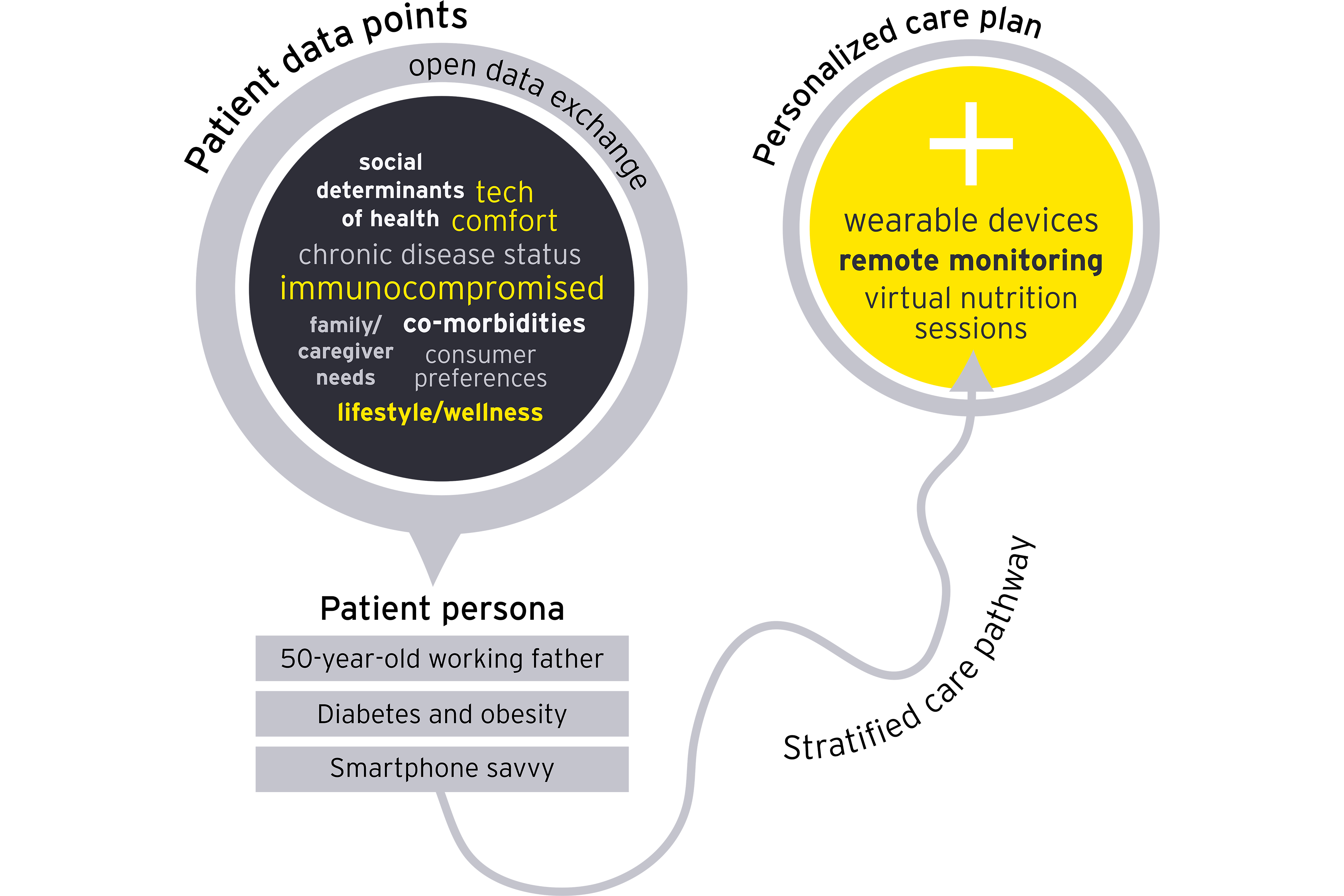
The first step in realizing the potential of integrated virtual and in-person care is knowing your patient pool. An analysis of areas with high utilization but low-acuity care can spotlight opportunities to shift care out of the hospital. Doing so increases capacity for those who truly need to be in an inpatient or emergency setting and allows clinicians to practice at the top of their license, improving their feelings of purpose so they can focus on in-person interactions with patients.
“When patients come to one of our services with a clinical challenge, we want to meet that challenge with the right capability,” said Dr. Bill Beninati, who helps lead TeleHealth Services, Patient Placement and Transfer, Life Flight, and Classic Air Medical, for Intermountain Healthcare. “We want all clinical leaders to be so capable and fluent in telehealth that when they're solving clinical problems, it's part of their toolkit.